Abstract
INTRODUCTION: AHUS is a rare thrombotic microangiopathy (TMA), classically defined as microangiopathic hemolytic anemia, thrombocytopenia, and end-organ damage caused by alternative complement pathway abnormalities. Complement amplifying conditions (CACs) have been demonstrated to provoke or be associated with the emergence of aHUS manifestations, but their presence has also been associated with longer time to treatment initiation despite similar clinical presentation. (Cunningham et al. ASH 2016) Prior to effective therapy, more than half of patients progressed to death or end-stage renal disease within one year. (Noris et al. CJASN 2010) Eculizumab (ECU), a monoclonal C5 inhibitor, was approved for the treatment of aHUS in 2011. (Legendre et al. NEJM 2013) Here we report the results of the largest retrospective, single center series in the literature to date of 52 patients diagnosed with aHUS treated with ECU.
METHODS: We performed a retrospective chart review of all patients diagnosed with aHUS who received at least one dose of ECU between December 2011 and February 2017 at MedStar Georgetown University Hospital.
RESULTS: Fifty three patients received at least one dose of ECU for the treatment of aHUS between December 2011 and February 2017. One patient received a single dose of ECU, but was later found to have an ADAMTS13 level <5% and was removed from further analysis.
CACs were identified in 71% of the 52 patients and 29% had de novo aHUS. Ninety percent of patients received ≥1 month of ECU and 40% remain on chronic ECU therapy through 15 February 2017. Of the 21 patients on chronic therapy, 67% had CACs and 33% did not. Of the 31 patients not currently known to be on therapy, 81% discontinued therapy or died and the treatment status was unknown in 19%. Six patients (12%) are deceased.
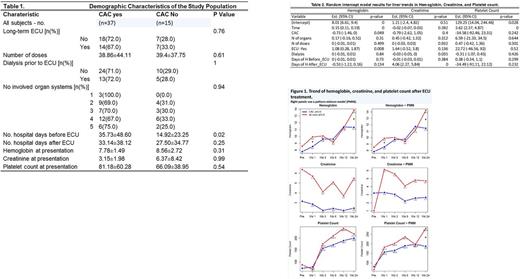
Forty three patients were diagnosed while inpatients. Patients with CAC-associated aHUS had more pre-treatment days in the hospital than patients with de novo aHUS (35.73 and 12.92 days, respectively, p = 0.02). The lengths of hospital stays after ECU initiation were similar: 33.1 and 27.5 days, respectively. Presenting organ system involvement and laboratory data, including hemoglobin, platelet count and creatinine, were similar. (Table 1.) When adjusted for other variables, mean hemoglobin at presentation was lower in patients with CACs (p = 0.049). (Table 2.) After ECU initiation, similar trends in improvement of hemoglobin, platelet count, and creatinine were observed. (Figure 1)
Hemodialysis (HD) rates prior to ECU initiation were similar regardless of CAC status. (Table 1.) Thirty five percent were started on HD either prior to or on the day of ECU initiation. Seventeen patients remained on HD one month post ECU, 14 of whom received ≥1 month of ECU. Eleven patients remained on HD ≥ 3 months post ECU, 6 /11 received ≥ 3 months of ECU, 3/11 received ≤ 3 months of ECU, and 2/11 were lost to follow-up. Three patients were on HD ≥1 month but ≤ 3 months; 1 remained on ECU through the 3 month time-point and two discontinued ECU after 4 and 5 weeks of therapy. Three patients on HD at 1 month were subsequently lost to follow-up.
Six patient deaths (12%) were observed during the period of follow-up: 5 of 37 patients with CACs (14%) and 1 of 15 (6%) with de novo aHUS. CACs observed in the patients who died were non-renal solid organ transplant in 2 patients, renal transplant, rheumatoid arthritis, and ulcerative colitis. These patients had documented TMA involvement of between 2-5 organ systems. Survival after ECU initiation ranged from 2 to 24 weeks in the CAC associated group. The single patient death in the de novo aHUS group occurred at 20 weeks of follow-up. Four of the 6 patients remained on ECU through the date of death, including the single observed death in the de novo aHUS group, and 2 patients discontinued ECU after 4 and 9 weeks.
CONCLUSION: In a single center non clinical trial setting both CAC associated and de novo aHUS can be effectively treated with ECU. CAC status did not affect presentation characteristics. CAC status did not correlate with hematologic or creatinine response to ECU therapy. Our results suggest a higher rate of death among the CAC-associated aHUS patient population perhaps reflecting a longer time to diagnosis. Most patients remain on long-term therapy, regardless of CAC status at the time of diagnosis.
Cunningham: TrueNorth therapeutics: Honoraria. Broome: TrueNorth Therapuetics: Honoraria; Alexion Pharmaceuticals: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal